Quetiapine
"Cheap quetiapine 300mg without a prescription, medications memory loss."
By: Karen Patton Alexander, MD
- Professor of Medicine
- Member in the Duke Clinical Research Institute

https://medicine.duke.edu/faculty/karen-patton-alexander-md
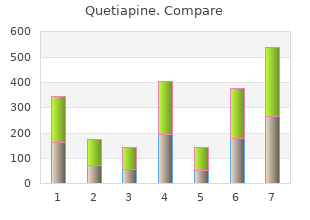
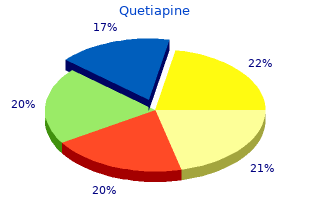
Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admis sion characteristics cheap quetiapine american express treatment tinea versicolor. Antiepileptogenesis and seizure prevention trials with antiepileptic drugs: meta-analysis of controlled trials cheap 300 mg quetiapine otc acne natural treatment. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to order genuine quetiapine line nail treatment play. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. The ability to heal will depend on many factors, including metabolic state and endogenous repair capacity of the brain. The cell and tissue level events in the brain can manifest as sensory, motor, cognitive, behavioral, affective, systemic, and/or somatic conditions. Heterogeneity stems from the variation in the inherent nature of a system and/or in the response to a changing state. Innate heterogeneity (nonchangeable): individual characteristics such as sex, age, stature, genetic variation, and neuroanatomic and musculoskel etal variations 2. Premorbid factors (potentially changeable): individual preexisting medi cal conditions or disease. Biomechanics of the causative event: magnitude and direction of force and acceleration, surface area of impact. Environmental heterogeneity at the time of the event: temperature, humid ity, head protection, impact surface, degree of anticipation C. Primary injury or biomechanical response: dependent on tissue mechani cal properties, tissue orientation, loading direction 2. Early secondary injury: complex cell signaling cascades dependent on type and number of cells affected, intrinsic cellular characteristics 3. Clinical intervention: variations in the time window to care and prehos pital protocols D. Postinjury heterogeneity (secondary injury, repair capacity, clinical management): 1. Repair capacity: innate and premorbid factors superimposed with the injury response and ability to stably repair. Force trans duction to the tissue and cells is not well understood because each loading event and individual is unique. Details of the biomechanical conditions around a trau matic insult are typically not known. Event Biomechanics: Load > Dynamic Head Response > Transduction to Brain > Brain Response 12 I. Core Concepts � Loading conditions: the forces, rates, and other parameters of the traumatic insult. Load is usually a combination of impact and inertial forces: � Impact load: Force resulting from a moving person striking a mass or obstruction, or a moving object or obstruction striking a person. Diffuse injury may result from the inertial load (especially high angular acceleration) and from the brain movement upon deceleration. The force produced by loading and subsequent head movement (accelera tion pattern) will be transduced to the brain tissue and the cell components. The lower the mass, the higher the acceleration must be to keep the force constant. The biomechanical response is a function of material properties and cell ori entation and will dictate the primary injury. Deformation (or strain) can be tensile (stretch), com pressive, and/or shear (note: the brain is especially vulnerable to shear strain). Primary damage may manifest in neurons, glial cells, and vascular cells as axonal stretching, membrane disruption, ion imbal ance, interruption in normal conduction and synaptic transmission, and glial damage (nano and microscale). Injury threshold: the insult level at which structural and functional compro mise or failure takes place; described using injury tolerance criteria. Development of tolerance criteria requires understanding of the relationship among traumatic insult, mechanical response of the brain tissue, and the resulting injury cascades and neuropathology. The following general cat egories of secondary injury processes are interrelated: A.
There should be a standardized intake buy quetiapine in united states online symptoms torn rotator cuff, such as the acute concussion evaluation [10] buy cheap quetiapine 50mg on-line medical treatment 80ddb, to purchase 200 mg quetiapine symptoms your having a girl ensure a comprehensive evaluation of symptoms. In addition, it is important to identify patient-perceived impact of head injury and goals for recovery. Frequently, the treatment applied is based on recommendations that have been successful in the relevant psychiatric and sleep disorder in the non-traumatic brain injury population [94]. The approach to treatment in patients with comorbid sleep and psychiatric dysfunction should address symptoms of both processes. In general, psychiatric medications in pediatrics are started with the lowest dosing and titrated slowly, as pediatric patients may be more susceptible to side effects of these medications [94�97]. The selection of medication is based on the psychiatric symptoms present (Table 6). Selective serotonin reuptake inhibitors are considered first-line treatment for anxiety and depression [94]. The approach to treating sleep�wake dysfunction is dependent on the specific sleep disorder present (Figures 1 and 2). Amitriptyline has also been subjectively reported by patients to help with sleep disorders by increasing their sleep duration, despite any statistical difference being shown [113]. Alternative therapies, such as acupuncture, have even demonstrated subjectively improved sleep quality, cognitive function, and the ability to taper sleep medication use [119]. Earlier recommendations include the importance of transition support including alerting school of injury and potential consequences, monitoring students for any increased needs, and offering assistance or adjusting requirements for a couple of weeks post injury [11]. Symptom checklists are not adequate screening tools for all potential psychiatric outcomes, which highlights the importance of the physician�s role in screening for psychiatric disorders and suicidal ideation post injury [26]. Discussion and Future Direction Traumatic brain injury is a signicant pediatric public health concern. This is evidenced by the features of post-concussive syndrome that can include evolving symptoms of physical, psychological, cognitive, and sleep�wake dysfunction. Increased comorbidity, such as co-occurrence of sleep�wake dysfunction and psychiatric illness, leads to more deleterious outcomes and a more protracted recovery. A multi-disciplinary approach is necessary to provide the comprehensive care necessary in these patients to optimize recovery. Perception of an injury and expectations for recovery can dramatically inuence patient outcomes [17]. Early incorporation of psychological support should be evaluated as a potential tool for improving outcomes in pediatrics. Adult studies have demonstrated benet of both pharmacological treatments and non-pharmacological treatments; however, there is still a signicant gap in knowledge when it comes to pediatric treatments. Clinical studies that partner with school systems that implement baseline cognitive assessments may help in lling this data void. In order to improve understanding of how sleep and psychiatric symptoms inuence recovery, longitudinal studies are needed. The effect of pediatric traumatic brain injury on behavioral outcomes: A systematic review. An investigation of the pre-injury risk factors associated with children who experience traumatic brain injury. Predictors of attention-decit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. Concussion As a Multi-Scale Complex System: An Interdisciplinary Synthesis of Current Knowledge. Prospective evaluation of the nature, course, and impact of acute sleep abnormality after traumatic brain injury. Outcomes 5 years post-traumatic brain injury (with further reference to neurophysical impairment and disability). Incidence of severe dysphagia after brain surgery in pediatric traumatic brain injury: A nationwide population-based retrospective study. Incidence, characteristics, and predictive factors for dysphagia after pediatric traumatic brain injury. Anxiety disorders in children and adolescents in the rst six months after traumatic brain injury. Long-term behavior problems following pediatric traumatic brain injury: Prevalence, predictors, and correlates.
Order quetiapine 100mg otc. 샤이니_상사병 (Symptoms by SHINee@Mcountdown 2013.10.10).
Brain tissue lactate elevations predict episodes of intracranial hypertension in patients with traumatic brain injury cheap 50mg quetiapine with mastercard treatment hyperkalemia. Temporal changes in cerebral tissue oxygenation with cerebrovascular pressure reactivity in severe traumatic brain injury discount quetiapine master card symptoms leukemia. Metabolic failure precedes intracranial pressure rises in traumatic brain injury: a microdialysis study best order for quetiapine medicine 003. Re-defining the ischemic threshold for jugular venous oxygen saturation-a microdialysis study in patients with severe head injury. Monitoring of autoregulation using intracerebral microdialysis in patients with severe head injury. Multiparametric analysis of cerebral substrates and nitric oxide delivery in cerebrospinal fluid in patients with intracerebral haemorrhage: correlation with hemodynamics and outcome. An assessment of dynamic autoregulation from spontaneous fluctuations of cerebral blood flow velocity: a comparison of two models, index of autoregulation and mean flow index. The human brain utilizes lactate via the tricarboxylic acid cycle: a 13C-labelled microdialysis and high-resolution nuclear magnetic resonance study. Spreading depolarizations and late secondary insults after traumatic brain injury. Brain tissue oxygen tension response to induced hyperoxia reduced in hypoperfused brain. Differential influence of arterial blood glucose on cerebral metabolism following severe traumatic brain injury. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Dynamic cerebral autoregulation: should intracranial pressure be taken into account Monitoring brain tissue oxygen tension in brain injured patients reveals hypoxic episodes in normal-appearing and in peri-focal tissue. Prediction of outcome utilizing both physiological and biochemical parameters in severe head injury. Acute lung injury is an independent risk factor for brain hypoxia after severe traumatic brain injury. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Lack of utility of arteriojugular venous differences of lactate as a reliable indicator of increased brain anaerobic metabolism in traumatic brain injury. Reactivity of brain tissue oxygen to change in cerebral perfusion pressure in head injured patients. Cerebral hemodynamic effects of acute hyperoxia and hyperventilation after severe traumatic brain injury. Online correlation of spontaneous arterial and intracranial pressure fluctuations in patients with diffuse severe head injury. Vestibulo-ocular monitoring as a predictor of outcome after severe traumatic brain injury. Fuzzy pattern classification of hemodynamic data can be used to determine noninvasive intracranial pressure. Continuous monitoring of jugular bulb oxygen saturation in comatose patients-therapeutic implications. Characterizing the dose-response relationship between mannitol and intracranial pressure in traumatic brain injury patients using a high-frequency physiological data collection system. Monitoring of cerebral metabolism: non-ischemic impairment of oxidative metabolism following severe traumatic brain injury. Intracranial multimodal monitoring for acute brain injury: a single institution review of current practices.
If the blood pressure while lying down is very high purchase discount quetiapine treatment quad tendonitis, then more than a 20 mmHg fall in systolic pressure may be required for the doctor to order cheap quetiapine on line medications 7 rights diagnose orthostatic hypotension buy quetiapine 300 mg low cost medicine naproxen 500mg. The level of the blood pressure, as well as levels of all the main numbers of the body, such as your temperature, your oxygen level, and your glucose level, are kept in check by reflexes. When your blood pressure falls, such as because of injection of 275 Principles of Autonomic Medicine v. The brain directs activation of the sympathetic noradrenergic system, which tightens the blood vessels, tending to bring the blood pressure back up. Orthostatic hypotension is a key sign of failure to tighten blood vessels reflexively by activation of the sympathetic noradrenergic system. In other words, orthostatic hypotension is a sign of sympathetic neurocirculatory failure. A fall in blood pressure when the patient stands up or is tilted head-up on a tilt table (orthostatic hypotension) is an important sign of failure of the sympathetic noradrenergic system. Many factors besides failure of the sympathetic noradrenergic system, however, can cause orthostatic hypotension. Indeed, in the American space program, a study of normal volunteers found that after prolonged bed rest with the head slightly down, healthy people can have orthostatic hypotension. It should not be surprising that elderly, bedridden patients also often have orthostatic hypotension. Orthostatic hypotension can also result from conditions that cause depletion of blood volume, such as heavy menstrual periods or gastrointestinal hemorrhage from a bleeding ulcer. Any of several drugs can do this, including tricyclics, monoamine oxidase inhibitors, and ganglion blockers. There are many causes of orthostatic hypotension besides sympathetic noradrenergic system failure. Doctors may have different opinions about the amount of orthostatic hypotension that is clinically significant. Normally the systolic blood pressure falls slightly during standing up, because the heart is ejecting less blood, and normally the diastolic pressure does not fall at all, because of the constriction of blood vessels in the body as a whole by way of the baroreflex and activation of the sympathetic noradrenergic system. Some people have a fall in blood pressure accompanied by lightheadedness as soon as they get up, but then the blood pressure comes up to normal. Most experts do not consider this to be orthostatic hypotension, because the fall in blood pressure 277 Principles of Autonomic Medicine v. Any of several diseases can produce orthostatic hypotension from sympathetic neurocirculatory failure. There are several other dysautonomias in which the patients cannot tolerate prolonged standing, even though they do not have persistent, consistent orthostatic hypotension. Much less commonly, chronic orthostatic intolerance can be a manifestation of arterial baroreflex failure. Orthostatic intolerance is not a sign, because it isn�t something an observer can measure objectively. And it isn�t a disease, although there are many diseases that produce orthostatic intolerance. A large proportion of patients with chronic fatigue syndrome have chronic orthostatic intolerance. The fact that there are many possible causes of orthostatic intolerance poses a challenge to doctors trying to come up with a diagnosis to explain orthostatic intolerance in a particular patient. A starting point in identifying a cause of orthostatic intolerance is to determine whether the patient has failure of the sympathetic noradrenergic system to regulate the heart and blood vessels correctly. In other forms of chronic orthostatic intolerance, the person does not have sympathetic neurocirculatory failure, and the 279 Principles of Autonomic Medicine v. Instead, the person feels dizzy or lightheaded during standing, even though the blood pressure is maintained. Orthostatic hypotension may or may not produce orthostatic intolerance, and orthostatic intolerance can occur without orthostatic hypotension. In the evaluation of a patient with chronic orthostatic intolerance in which the patient does not have evidence of sympathetic neurocirculatory failure, doctors often prescribe a tilt table test.
References:
- https://www.dshs.wa.gov/sites/default/files/BHSIA/dbh/documents/Bestpracreport.pdf
- https://www.temple.edu/boyer/academicprograms/music-therapy/documents/ENVISIONING_THE_FUTURE.pdf
- https://www.ssa.gov/policy/docs/ssb/v70n3/ssb-v70n3.pdf