Plendil
"Purchase on line plendil, heart attack xbox."
By: Karen Patton Alexander, MD
- Professor of Medicine
- Member in the Duke Clinical Research Institute

https://medicine.duke.edu/faculty/karen-patton-alexander-md
Infants with congenital rubella or cytomegalovirus infection with microcephaly have a poor outcome buy plendil australia blood pressure for children, with a handicap rate >50% buy plendil 2.5mg blood pressure record chart. Fewer than half of twin pregnancies diagnosed with ultrasonography during the first trimester are finally delivered as twins cheap 2.5 mg plendil overnight delivery blood pressure formula, a phenomenon that has been termed vanishing twin. In addition, routine screening for maternal alpha-fetoprotein will identify about half of the pregnancies with multiple gestations at an early gestational age. The incidence of monozygotic twinning is remarkably constant at 3-5 per 1000 pregnancies, whereas the rate for dizygotic twinning varies from 4-50 per 1000 pregnancies. The rate of monozygotic twinning is considered a chance phenomenon, whereas dizygotic twinning results from multiple ovulation, shows wide ethnic variability, and may have a familial tendency. The incidence of dizygotic twinning increases with a family history of twins, maternal age (peak at 35-39 years), previous twin gestation, increasing parity, maternal height, fecundity, social class, frequency of coitus, and exposure to exogenous gonadotropins (20-40% incidence) and clomiphene (6-8% incidence). Ethnic background (African Americans > Caucasians > Asians) is a preconception risk factor for multiple gestation. Over the last two decades, there has been a striking increase in the frequency of pleural births. Between 1980 and 1994, there was a 42% increase in the number of twin births, and the twin birth rate (ie, the number of twin births to total live births) increased 30% from 18. The rate of triplet births has escalated more rapidly, increasing 100% between 1980 and 1989. White women, especially those >30 years of age, accounted for the bulk of this increase. It is likely that much of this increase stems from the use of ovulation-inducing drugs for the treatment of infertility (Kiely et al, 1992). By 1997, the use of assisted reproductive technology accounted for more than 40% of triplets born in the United States (Schieve et al, 2002). Placental examination affords a unique opportunity to identify two thirds to three fourths of monozygotic twins at birth. Twin placentation is classified according to the placental disk (single, fused, or separate), number of chorions (monochorionic or dichorionic), and number of amnions (monoamniotic or diamniotic) (Figure 70-1). In 70% of monozygotic twin pregnancies, the placentas are monochorionic, and the possibility exists for commingling of the fetal circulations. Twin gestations are associated with an increased frequency of anomalies of the placenta and adnexa; for example, a single umbilical artery or velamentous or marginal cord insertion (6-9 times more common with twin gestation). Intrapartum fetal distress from cord compression and fetal hemorrhage from associated vasa previa are potential problems with velamentous insertion of the cord. If doubt exists on gross inspection of the dividing membranes, a transverse section should be studied. The zygosity of twins of the same sex with dichorionic membranes cannot be immediately known. Although perinatal mortality rates for singleton pregnancies have continued to fall during the last decade, there has been little change in mortality rates for multiple pregnancies. For twin gestations, the fetal mortality rate is 4%, the neonatal mortality rate 7. The perinatal death rate for twins is 9 times the rate for first-born singletons and 11 times the rate for second-born singletons. The mortality rate for monoamniotic twins is highest (50-60%), largely because of cord entanglement. Monozygotic twins have a perinatal mortality and morbidity rate that is 2-3 times that of dizygotic twins. Diamniotic monochorionic twins have a mortality rate of 25%, and dichorionic twins, a mortality rate of 8. Approximately 10% of preterm deliveries are twin gestations, and they account for 25% of perinatal deaths in preterm deliveries. Death of one fetus may affect the outcome of the survivor profoundly or minimally (Dudley & Dalton, 1986).
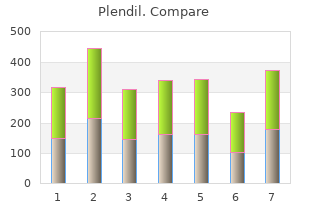
Current evidence does not support a spe cific concentration of glucose that can discriminate normal from abnormal or can potentially result in acute or chronic irreversible neurologic damage purchase plendil overnight delivery blood pressure medication cialis. Early identification of the at-risk infant and institution of prophylactic measures to buy 2.5 mg plendil amex blood pressure chart hospital prevent neonatal hypoglycemia are recommended as a pragmatic approach despite the absence of a consistent definition of hypoglycemia in the literature buy discount plendil blood pressure medication restless leg syndrome. The following section describes the screening of neonatal hypoglycemia in at-risk late preterm (born between 34 0/7 weeks and 36 6/7 weeks of gesta tion) and term infants. Routine screening and monitoring of blood glucose concentration is not needed in healthy term newborns after an entirely normal pregnancy and delivery. Blood glucose concentration should only be measured in term infants who are known to be at risk or who have clinical manifestations. Neonatal hypoglycemia occurs most commonly in infants who are small for gestational age, infants born to mothers who have diabetes, and late preterm infants; whether otherwise healthy infants who are large for 300 Guidelines for Perinatal Care gestational age are at increased risk is uncertain, although this is assumed for practical reasons because it is difficult to exclude maternal hyperglycemia or diabetes. The clinical signs of neonatal hypoglycemia are not specific and include a wide range of local or generalized manifestations that are common in sick neonates, including jitteriness, cyanosis, seizures, apneic episodes, tachy pnea, weak or high-pitched cry, floppiness or lethargy, poor feeding, and eye rolling. It is important to screen for other possible underlying disorders (eg, infection) as well as hypoglycemia. Coma and seizures may occur with pro longed neonatal hypoglycemia (plasma or blood glucose concentrations lower than 10 mg/dL range) and repetitive hypoglycemia. Because avoidance and treatment of cerebral energy deficiency is the principal concern, greatest atten tion should be paid to neurologic signs. Plasma or blood glucose concentration should be measured as soon as possible (minutes, not hours) in any infant who manifests clini cal signs compatible with a low blood glucose concentration. At-risk infants should be fed by 1 hour of age and screened 30 minutes after the feeding. Glucose screening should continue until 12 hours of age for infants born to mothers with diabetes and those who are large for gestational age, and until 24 hours of age for late preterm and small for gestational age infants. At-risk asymptomatic infants should be fed every 2�3 hours and screened before each feeding. The target plasma glucose concentration is greater than or equal to 45 mg/dL before feedings. Management of infants who do not achieve target glucose levels is discussed in Chapter 9. When neonatal hypoglycemia is suspected, the plasma or blood glucose concentration must be determined immediately by using one of the laboratory enzymatic methods (eg, glucose oxidase, hexokinase, or dehy drogenase method). Although a laboratory determination is the most accurate method of measuring the glucose concentration, the results may not be available quickly enough for rapid diagnosis of neonatal hypoglycemia, which thereby delays the initiation of treatment. Bedside reagent test-strip glucose analyzers can be used if the test is performed carefully and the physician is aware of the limited accuracy of these devices. Because of limitations with rapid bedside methods, the blood or plasma glucose concentration must be confirmed by laboratory testing ordered stat. Treatment of suspected neonatal hypoglycemia should not be postponed while waiting for laboratory confirmation. Most jaundice is benign, but because of the potential toxicity of bilirubin, newborns must be monitored to identify those who might develop severe hyperbilirubinemia and, in rare cases, acute or chronic bilirubin encephalopathy. Based on a consensus of expert opinion and review of available evidence, universal predischarge bilirubin screening is rec ommended and can be performed by measuring total serum bilirubin levels at the time of routine metabolic screening or measuring transcutaneous bilirubin levels and plotting the result on an hour-specific nomogram to determine the risk of subsequent hyperbilirubinemia that will require treatment. Before discharge it is recommended that a systematic assessment for the risk of severe hyperbilirubinemia be made, a plan for treatment be developed (when indicated), and early follow-up after discharge be arranged based on the risk assessment (see also �Hyperbilirubinemia� in Chapter 9). Each nursery should develop policies and procedures for hyperbilirubinemia screening. These poli cies should consider the following elements: � Promotion and support of successful breastfeeding � Protocols for identification and evaluation of hyperbilirubinemia � Provision for measurement of the total serum bilirubin or transcutane ous bilirubin concentration in infants who are jaundiced in the first 24 hours � Recognition that visual estimation of the degree of jaundice can lead to errors, especially in darkly pigmented infants � Interpretation of all bilirubin levels according to the infant�s age in hours (Fig. Nomogram for designation of risk in 2,840 well newborns at 36 or more weeks of gestational age with birth weight of 2,000 g or more or 35 or more weeks of gestational age and birth weight of 2,500 g or more based on the hour-specific serum bilirubin values. Developmental dysplasia of the hip includes frank dislocation (luxation), partial dislocation (subluxation), instability wherein the femoral head comes in and out of the socket, and an array of radiographic abnormalities that reflect inadequate for mation of the acetabulum. The term developmental more accurately reflects the biologic features of hip dysplasia than does the term congenital, because not every dislocated hip is detectable at birth and hips continue to dislocate throughout the first year of life. The two maneuvers for assessing hip stability in the newborn are the 1) Ortolani test and 2) Barlow test. The Ortolani test elicits the sensation of the dislocated hip reducing, and the Barlow test detects the unstable hip dislocating from the acetabulum.
Necessary treatment without consent is to plendil 10 mg lowest price heart attack young square be provided to generic plendil 10 mg overnight delivery blood pressure chart for 80 year old woman a psychotic patient only in a medical emergency plendil 2.5mg for sale heart attack feat sen city. For a patient who is psychotic, information disclosure may be permitted by law. Once such a relationship arises, the physician is required to attend to the patient attentively, with continuity, and to exercise reasonable care, skill, and judgment (until the relationship is ended through an appropriate process). Duty of care for a psychotic patient arises out of the doctor/patient relationship. Once such a relationship has been established, the physician is required to attend the patient attentively, with continuity, and to exercise reasonable care, skill, and judgment until the relationship is ended trough an appropriate process. Patients with psychotic disorders may choose to discontinue medication, therapy, or both. Discuss these issues with the patient and with those that act on behalf of the patient. Carotid, radial, femoral, posterior tibial, and dorsalis pedis pulses should be examined routinely on both sides, and differences, if any, in amplitude, contour, and upstroke should be ascertained. Aortic disease (dissection, aneurysm, coarctation, supra/valvular aortic stenosis) c. Tachycardia, sinus (>100/minutes) (fever/sepsis, hyperthyroid, volume depletion/hypotension/shock/heart failure, anemia, hypoxemia, drugs) b. Intrinsic to heart (infiltrative diseases, collagen diseases, open heart surgery) iii. Extrinsic (vagal activity, drugs, hypothyroid, hypothermia, potassium abnormal) c. Objectives 2 Through efficient, focused, data gathering: � Examine brachial arterial pulse to assess rhythm, volume and consistency of peripheral vessels. Define laminar and turbulent flow and explain that turbulence may be produced by an increase in velocity (due to either geometric changes such as narrowing or increased flow rate). If only one pupil is fixed to light, it is suspicious of the effect of mydriatics. Impaired pupil dilatation (Horner syndrome) (hypothalamus/brain stem/spinal cord lesions) 3. Bilateral (diabetes, syphilis, midbrain lesion, hydrocephalus, factitious) Key Objectives 2 Determine whether there has been previous ocular inflammation, trauma, loss of vision, or eye pain in order to begin ruling out local disorders. Objectives 2 Through efficient, focused, data gathering: � Differentiate clinically between the various mechanisms of pupil abnormalities. Objectives 2 Through efficient, focused, data gathering: � Determine disease duration, recent onset of discoloured urine, decrease or no urine output, history of fluid loss, history of urinary tract obstruction, medications. Identify the determinants of single nephron glomerular filtration rate (surface area/permeability of glomerular basement membrane, hydrostatic pressure gradient between glomerular capillary and Bowman space, oncotic pressure gradient between glomerular capillary and Bowman space). Physicians must realise that patients with chronic renal failure have unique risks and that common therapies may be harmful because kidneys are frequently the main routes for excretion of many drugs. Post-renal causes (obstructive nephropathy) Key Objectives 2 Determine which patients with elevated serum creatinine levels have chronic rather than acute renal failure, and communicate as early as possible to such patients that progression to chronic renal failure may be avoided or delayed with conservative management. Objectives 2 Through efficient, focused, data gathering: � Identify patients at risk for chronic renal failure; ask about diabetes, hypertension, heart failure, past renal findings, and family history of kidney disease. Primary care physicians may be part of the process of withholding dialysis by not referring patients to nephrologists for evaluation for possible dialysis. For example, in one study, it was found 25% of primary care physicians had effectively withheld dialysis for at least one patient because of non-referral to a nephrologist. The most common reasons cited by the physicians were end-stage heart, liver, or lung disease, old age, and patient refusal. Ethical principles supporting the right of individuals who are competent to withdraw from dialysis or to refuse the initiation of dialysis include the principle of autonomy and the rights of self-determination and privacy. For example, continued life on dialysis for some patients (such as those in intractable pain) would impose an unfavorable balance between benefit and burden. All patients have the personal and legal right to refuse treatment, since any such informed decision involves the expression of self-determination, independence, and autonomy. Informed consent emanates from the right to privacy and holds that patients may refuse medical care. This right is based upon the presumption of full and honest informed consent, which includes: 1.
Mitral valve prolapse is not considered a lesion that ever needs infective endocarditis prophylaxis purchase plendil toronto prehypertension hypertension. In patients who have one of the high-risk conditions (see Box 7-3) and an established infection that could result in bacteremia discount plendil 5mg with visa blood pressure and stroke, such as chorioamnionitis or pyelonephritis generic 5 mg plendil with visa causes 0f hypertension, the underlying infection should be treated to prevent infec tion or sepsis, but specific additional endocarditis prophylaxis is not recom mended. For women not already receiving intrapartum antibiotic therapy for another indication that would also provide coverage against endocarditis, sin gle-dose antibiotic regimens for endocarditis prophylaxis can be administered as close to 30�60 minutes before the anticipated time of delivery as is feasible. Multiple-dose combination regimens are no longer indicated or recommended for prophylaxis. Clinically, endome tritis is characterized by fever, uterine tenderness, malaise, tachycardia, abdomi nal pain, or foul-smelling lochia. Of these, fever is the most characteristic and may be the only sign early in the course of infection. Risk factors for postpar tum endometritis include cesarean delivery, prolonged rupture of membranes, Obstetric and Medical Complications 253 prolonged labor with multiple vaginal examinations, intrapartum fever, and lower socioeconomic status. Prophylaxis Against Postcesarean Infection the single most important risk factor for infection in the postpartum period is cesarean delivery. Antimicrobial prophylaxis is recommended for all cesarean deliveries unless the patient is already receiving an antibiotic regimen with appropriate coverage (eg, for chorioamnionitis), and such prophylaxis should be administered within 60 minutes before the start of the cesarean delivery. When this is not possible (eg, need for emergent delivery), prophylaxis should be administered as soon as possible after the incision is made. A single dose of a targeted antibiotic, such as a first-generation cephalo sporin, is the first-line antibiotic of choice, unless significant drug allergies are present. For women with a history of a significant penicillin or cephalosporin allergy (anaphylaxis, angioedema, respiratory distress, or urticaria), a single-dose combination of clindamycin with an aminoglycoside is a reasonable alternative choice for cesarean delivery prophylaxis. After a single 1-gram intravenous dose of cefazolin, a therapeutic level is maintained for approximately 3�4 hours. Patients with lengthy sur geries or those who experience excessive blood loss should receive an additional intraoperative dose of the antibiotic used for preincision prophylaxis. A woman with postpartum fever should be evaluated by pertinent history, physical exam ination, blood count, and urine culture. Blood cultures rarely influence thera peutic decisions but could be indicated if septicemia is suspected. Cervical, vaginal, or endometrial cultures need not be routinely performed because the results might not indicate the infecting organism. Principles for managing postpartum endometritis are as follows: � Parenteral, broad-spectrum antibiotic treatment should be initiated according to a proven regimen and continued until the patient is afebrile. A combination of clindamycin and gentamicin, with the addition of ampicillin in refractory cases, is recommended for cost-effective therapy. If fever persists beyond antibiotic treatment for 24�48 hours, a search for alternative etiologies, including pelvic 254 Guidelines for Perinatal Care abscess, wound infection, septic pelvic thrombophlebitis, inadequate antibiotic coverage, and retained placental tissue, should be performed. Maternal Hemorrhage Hemorrhage remains one of the leading causes of maternal mortality world wide. One half of all maternal deaths occur within 24 hours of delivery and most commonly from excessive bleeding. Facilities that provide labor and delivery services should be prepared to manage maternal hemorrhage. Proper preparation and resources to manage maternal hemorrhage in a timely manner can be lifesaving. Policies to ensure the rapid availability of blood products for transfusion in the event of hemorrhage must be in place. Criteria of an esti mated blood loss of greater than 500 mL after a vaginal delivery or 1,000 mL after cesarean delivery are often used, but the average volume of blood lost at delivery can approach these amounts. Symptoms of hypotension, pallor, and oliguria typically do not occur until blood loss is substantial. Risk factors for excessive bleeding include prolonged, augmented, or rapid labor; history of postpartum hemorrhage; episiotomy, especially mediolateral; preeclampsia; overdistended uterus (macrosomia, twins, or hydramnios); operative delivery; Asian or Hispanic ethnicity; and chorioamnionitis.
Cheapest plendil. Blood Pressure Control Yoga | Yoga For Blood Pressure Control | Blood Pressure | Yoga In Telugu.
References:
- http://www.mbaa.com/meetings/archive/Documents/2008WBCprogbook.pdf
- http://labs.psychology.illinois.edu/~ediener/Documents/Diener-Chan_2011.pdf
- https://www.aafp.org/afp/2012/1015/p734.pdf